Hadad and Ohio State team seek deadly chemical nerve agent antidotes


An airman uses a nerve agent treatment on a simulated infected airman during a chemical, biological, radiological, nuclear and explosive training exercise. (U.S. Air Force photo/Samuel King Jr.)
In February 2017, North Korean leader Kim Jong-un’s half-brother, Kim Jong-nam, was assassinated in a Malaysian airport. Before having a seizure and dying en route to the hospital, he reported to airport officials that a woman had wiped a damp cloth across his face.
Kim Jong-nam was poisoned by VX, a toxin in a group of organophosphorus (OP) compounds considered chemical weapons that also include sarin, soman and Novichok agents. These poisons are extremely potent and have few options for treatment, according to the U.S. military, often “causing effects within seconds and death within minutes.”
To help confront that threat, the scientific research institute MRIGlobal and the Defense Threat Reduction Agency, part of the U.S. Department of Defense, awarded Ohio State $5,321,558 over the next five years to develop safe, drug-like organic molecules that have broad-spectrum activity to treat chemical nerve agent poisoning.
Christopher Hadad, professor in the Department of Chemistry and Biochemistry, leads the team alongside Craig McElroy, research assistant professor in the College of Pharmacy, and Christopher Callam, (associated) associate professor of chemistry and biochemistry. Together, they’re tackling a challenge that has thwarted researchers since such OP nerve agents were invented.
OP compounds have a long history of being used as tools of assassination and chemical warfare. Sadam Hussain used a cocktail containing tabun and sarin to kill Kurdish people in 1988 during the Iran–Iraq War. Syrian President Bashar Assad's regime used sarin on multiple occasions during the country’s civil war. In 2018, former Russian military intelligence officer and double agent Sergei Skripal and his daughter were poisoned by a Russian-developed Novichok agent. In 1995, members of a cult released sarin on the Tokyo metro in an act of domestic terrorism, killing 12 and injuring more than 1,000 others. Less toxic versions of OP compounds, often used as pesticides, account for around 200,000 suicides a year, primarily in developing countries.
“A new therapy for organophosphorus poisoning has not been approved in the U.S. since the early 1980s, and people are still dying every year from toxic exposures to these nerve agents and pesticides,” Hadad said.
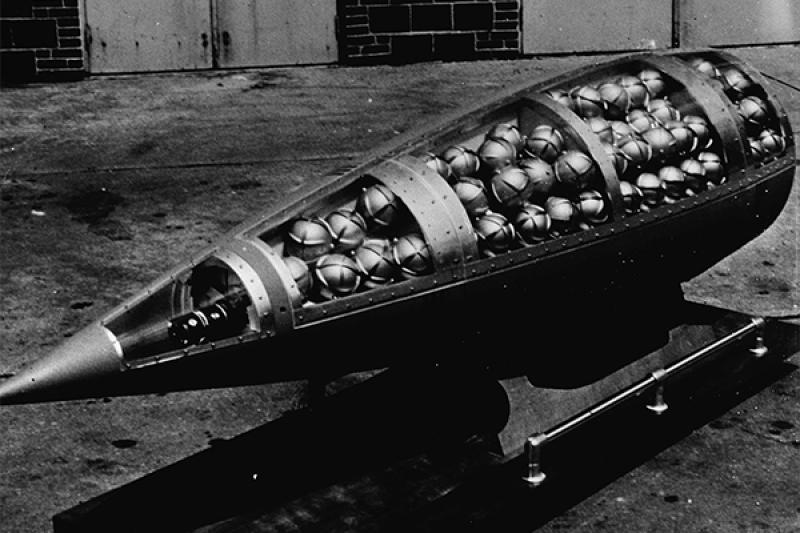
An U.S. M190 Honest John chemical warhead section containing demonstration sarin bomblets, likely from the 1960s. (U.S. Army)
OP compounds work by disrupting the body’s ability to regulate its peripheral and central nervous systems. The body uses a neurotransmitter called acetylcholine to communicate from nerve to nerve and from nerve to muscle. When acetylcholine binds to the receiving nerve or muscle, it sends a signal for that nerve or muscle to do its job — to turn “on,” so to speak. Then, an enzyme called acetylcholinesterase breaks down acetylcholine, turning the nerve or muscle “off” until it receives a new signal.
However, when an organophosphorus compound attaches to an acetylcholinesterase enzyme, the enzyme becomes inhibited and is unable to break down acetylcholine. The resulting buildup of acetylcholine causes hyperactivity in parts of the body and can have severe consequences.
Excessive accumulation of acetylcholine can cause cramps, increased salivation, muscular weakness and twitches, paralysis, diarrhea and blurry vision. Inhalation exposure to an OP compound can cause the diaphragm to lock up and the victim to suffocate. If the toxin gets into the blood and heart, the heart can beat erratically, causing a heart attack. If it reaches the brain, it can cause seizures and a coma.
People have tried to develop therapies for the aged form of acetylcholinesterase, generated by exposure to these organophosphorus compounds, for about 70 years, and no one was successful,” Hadad said. “It’s a big toxicological problem.”
Additionally, it takes shockingly little of some of these chemical agents to kill a person. A fatal dose of VX for an average male human, for example, would be just enough to fill in two pillars of the Lincoln Memorial on the back of a penny, Hadad said.
With that being said, around 80% of a person’s acetylcholinesterase can be inhibited without showing physiological effects.
“So we think if we can recover at least 20%, you probably will survive the exposure,” Hadad said.
Acetylcholinesterase goes through two phases when it binds with an OP compound. First, it makes what’s called the inhibited form of acetylcholinesterase. The enzyme is unable to bind to acetylcholine but can still be reactivated and returned to its native form.
However, Hadad said, “if you wait long enough, this inhibited form shifts into a new form called the aged form,” and the aged form is much more difficult to resurrect back to the native form.
The shift from inhibited to aged depends on the agent involved. A VX-inhibited enzyme will age in 48 hours. But soman ages in two to six minutes, making it particularly concerning for the U.S. military, Hadad said.
“People have tried to develop therapies for the aged form of acetylcholinesterase, generated by exposure to these organophosphorus compounds, for about 70 years, and no one was successful,” Hadad said. “It’s a big toxicological problem.”

U.S. soldiers patrol through yellow smoke simulating chemical, biological, radiological exposure during combat. (U.S. Navy photo/Todd Frantom)
Of the handful of medications used to treat the toxin’s impacts, only one actually addresses the OP compound, cleaving it from the acetylcholinesterase and restoring the enzyme’s activity.
However, that medication, pralidoxime, doesn’t work on the aged form. It also doesn’t work with every OP compound, it must be administered in massive doses, and it doesn’t cross the blood-brain barrier, so it can’t help with any toxin that has reached the brain. Hadad’s team is on its way to develop a treatment without those disadvantages.
“We’ve already shown that we have the first compounds ever that can take the aged form back to native, and we have shown that our compounds also can take the inhibited form back to native and can cross the blood-brain barrier,” Hadad said.
Now, the team needs to figure out how to make those compounds work faster and in lower doses.
In addition to acetylcholinesterase, the team is working with another enzyme, butyrylcholinesterase. Butyrylcholinesterase reacts with OP compounds the same way, but it doesn’t have a known essential function in the body, so it acts like a sponge, Hadad said. The more butyrylcholinesterase someone has, the more OP toxin their body can handle.
"If we could do the same thing with butyrylcholinesterase, take the inhibited form back to the native or take the aged form back to the native, we essentially could allow you to tolerate a higher dose,” Hadad said. “And if we can reactivate both the inhibited form and resurrect the aged form of both enzymes, then we’re essentially giving a multi-headed opportunity to improve your ability to survive a lethal dose of an organophosphorus agent.”
Hadad and his team are testing various families of similar compounds to try to identify which ones are promising. They’re combing through chemical frameworks to see which have the best activity, and they’re using those data to try to identify trends — which structures do reactivation or resurrection better. From there, they’ll send the best compounds to MRIGlobal for further testing.
“One of the things we don't know yet is whether we could get one compound, or maybe a few compounds, that have broad capacity to be able to do different sorts of things,” Hadad said.
He says the team is hoping they won’t have to create different treatments for each OP compound, but that may be the case since each OP compound has its own unique structure.
Regardless of the final number, such compounds will have great value to the Department of Defense and will provide a true countermeasure for OP poisoning to the warfighter and first responder in a military setting or on a subway.
